Background
Ruxolitinib, a Janus Kinase inhibitor, was approved in 2011 for the treatment of primary myelofibrosis (PMF) and has shown improved survival since its introduction. However, there are reports of possible cardiotoxicity linked to the medication. 1,2 Previous studies have shown that cardiovascular disease (CVD) was the third most common cause of death in PMF. 3 Given that patients with PMF may need therapy for several years, the cardiovascular safety profile of ruxolitinib has been the subject of increased scrutiny. Our goal was to compare the cardiovascular-related mortality (CVM) risk in patients with PMF in the pre-ruxolitinib (pre-Rux) and ruxolitinib (Rux) eras.
Methods
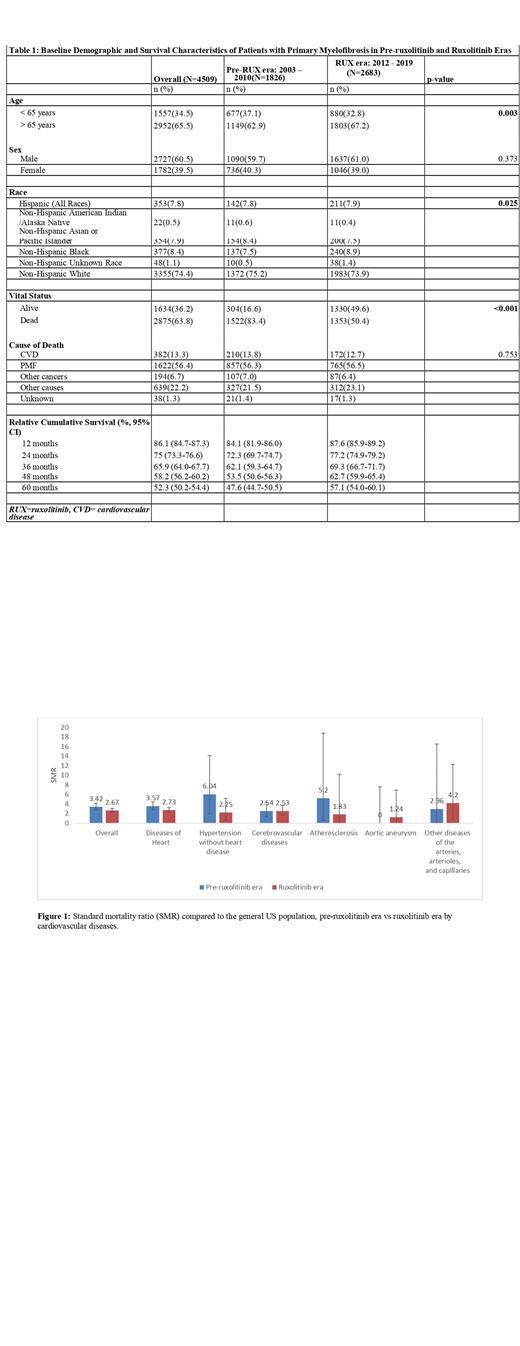
Using the Surveillance, Epidemiology, and End-result (SEER) Research Plus Data, 17 Registries and Multiple Primary Standardized Incidence Ratio (MP-SIR) registries (2000 - 2020), a retrospective study of patients diagnosed with PMF between 2003 and 2019 was conducted. This period was split into the pre-Rux (2003-2010) and post-approval Rux eras (2012-2019) and compared the standard mortality ratios (SMRs) of CVD in both periods. SMR was expressed as the ratio of cardiovascular deaths observed in PMF to those expected in the general population. Descriptive statistics (frequencies) were compared with Chi-square. The Kaplan-Meier method was used to estimate cumulative relative survival (CRS), and the sub-distribution hazard model for competing risk analysis was used to predict CVM; the significance test was set at <0.05.
Results
4,509 patients with PMF were identified between the two study periods (2003-2010 and 2012-2019). As shown in Table 1, a higher proportion of older patients aged 65+ years (67.2% vs. 62.9%, p=0.003) and Non-Hispanic Blacks (8.9% vs. 7.5%, p=0.025) were diagnosed in the Rux era. More patients were alive (49.6% vs. 16.6%, p<0.001), and 5-year CRS was higher in the Rux period (57.1% vs. 47.6%). There was no significant difference in the proportion of deaths due to cardiovascular disease between the two periods. Compared to the general population, patients with PMF had a higher overall CVM independent of the era of diagnosis ( Figure 1). However, there was a decrease in SMR of overall CVD in the post-Rux period (SMR=2.67; 95% CI: 2.28-3.10) compared to the pre-Rux (SMR: 3.42; 95% CI: 2.79-4.15). In terms of specific CVD, the SMRs of diseases of the heart, hypertension without heart diseases, and cerebrovascular disease were higher in the pre-RUX period compared to the Rux era, where SMR was higher only in diseases of the heart, which was still lower than the pre-Rux period (SMR: 2.73 [2.28-3.24] vs. 3.57 [2.84-4.44]). There was no significant difference in the mortality risk from other CVD compared to the general population in both periods. On multivariate analysis, after adjusting for age, sex, race and era of diagnosis, factors associated with reduced odds of CVM were diagnosis of PMF in the RUX era ( HR=0.76; 95% CI: 0.61-0.94, p=0.012), female gender ( HR=0.72; 95% CI: 0.58-0.89, p=0.002) and younger age (<65 years, HR= 0.12; 95% CI: 0.09-0.17, p<0.001. Non-Hispanic Black race was an independent predictor of increased CVM.
Conclusion
The risk of CVM in PMF compared to the general population did not seem to have increased in the era following the approval of ruxolitinib. The SMRs for overall and some specific cardiovascular diseases appear to be lower in the ruxolitinib era compared to the period before its approval. Lastly, the period following the introduction of ruxolitinib was associated with reduced death from cardiovascular diseases. Hence, ruxolitinib may have had some mortality benefits from cardiovascular disease in PMF; however, further studies are needed to examine and validate this observation.
References
1. Verstovsek S, Mesa RA, Gotlib J, Gupta V, DiPersio JF, Catalano JV, et al. Long-term treatment with ruxolitinib for patients with myelofibrosis: 5-year update from the randomized, double-blind, placebo-controlled, phase 3 COMFORT-I trial. J Hematol Oncol 10: 55, 2017. 2. Vannucchi A.M., Kiladjian J.J., Griesshammer M., Masszi T., Durrant S., Passamonti F., et al. Ruxolitinib versus standard therapy for the treatment of polycythemia vera. N Engl. J. Med. 2015; 372:426-435. doi: 10.1056/NEJMoa1409002. 3. Garmezy B, Boonstra PS, Kandarpa M, Talpaz M. The Relationship between Cause of Death in Myelofibrosis and the Dynamic International Prognostic Scoring System. Blood. 2017 Dec 8; 130:2929.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal